Prostate Specific Antigen (PSA) Test
PSA or prostate specific antigen is a test which is used in clinical practice to quantify the amount of prostate specific antigen in the blood for diagnostic or prognostic purposes. PSA is a normal protein that is released in the blood of males as part of the normal functioning of the prostate gland. The total serum levels of PSA are generally low in adult healthy men; however, with advancing age and physiological changes in the glandular matrix, the serum levels may rise slightly in the blood. It is imperative to keep in mind that PSA levels are not hazardous per se and carries only diagnostic value.
Conditions That Are Associated With Significantly High Levels of PSA?
High levels of prostate specific antigen may be physiological or pathological.
Physiologically high levels of PSA are observed in following conditions. It is noteworthy that the rise is only transient and normalizes spontaneously within a few hours.
- After ejaculation
- Sexual activity
- Genital injury
Pathologically high levels of PSA are observed in:
- Prostatitis (inflammation of prostate gland)
- Prostate cancer. Why PSA is done
What Are Indications of PSA Test?
 Prostate specific antigen test is performed in adult males to evaluate the functions of prostate gland. A few indications are:
Prostate specific antigen test is performed in adult males to evaluate the functions of prostate gland. A few indications are:
- Screening test to diagnose prostate cancer; the levels are abnormally high in case of a cancerous growth. PSA test is generally followed by biopsy of prostate gland to confirm the findings of physical test and serum investigation.
- If an adult male is manifesting symptoms of prostate inflammation with no findings on normal physical examination.
- As a prognostic test after the surgical removal of prostate gland. Persistently high PSA levels after surgery are suggestive of incomplete tumor resection or concealed masses elsewhere.
What Are Some Adverse Effects of PSA Test?
The PSA test is generally safe and is not associated with major complication or adverse effects. Some common issues are:
- A small bruise may appear on the site (vein) from where the blood is taken for analysis. This problem can be overcome by applying mild pressure over the injection site.
- Phlebitis (inflammatory damage to the vein) is a rare complication that is seen in some patients. Application of a warm compress can resolve phlebitis without needing any other intervention.
- Patients suffering from bleeding disorders may experience prolonged bleeding. Ingestion of blood thinning agents such as aspirin should be avoided before undergoing PSA test.
Reference Ranges/Results
Reference ranges or normal values for prostate specific antigen tests are discussed below, it is to be noted that these ranges may vary from laboratory to laboratory.
Normal Prostate Specific Antigen ranges for men:
- For men of age 40-49: 0-2.5 nanograms/liter or 0-2.5 micrograms/liter
- For men of age 50-59: 0-3.5 nanograms/liter or 0-3.5 micrograms/liter
- For men of age 60-69:0-4.4 nanograms/liter or 0-4.5 micrograms/liter
- For men of age 70-79: 0-6.5 nanograms/liter or 0-6.5 micrograms/liter.
Levels higher than 8 nanograms/liter are suggestive of prostate malignancy. TRUS (Trans-rectal ultrasound) and prostate biopsy can be performed to confirm the diagnosis.
Free Prostate Specific Antigen Detection For Prostate Cancer Prognosis:
 Free prostate specific antigen levels are assessed for the estimation of risk of cancer growth in the prostate. A lower level of free PSA is suggestive of a higher likelihood of developing prostate malignancy.
Free prostate specific antigen levels are assessed for the estimation of risk of cancer growth in the prostate. A lower level of free PSA is suggestive of a higher likelihood of developing prostate malignancy.
- If the levels are 25% higher than the normal baseline value, the risk of developing prostate malignancy is 8%.
- In case of 20-25% free PSA, the risk is 16%
- With levels between 15-20% the risk of malignancy rises to 20%
- If the levels are 10-15% the risk is 28%
- If the levels of free PSA are 0-10% then the probability of developing cancer increases to 56%.
Factors That May Affect The Outcome of The Test
The results of prostate specific antigen may appear false positive in some conditions. It is highly recommended to ask about the following scenarios in the history from the patient before conducing the test:
- No history of recent ejaculation
- Recent catheter use is associated with false positive results
- History of urinary tract infection should be confirmed
- Digital rectal exam should be avoided just before the test
- Certain medications used for cancer therapy can also alter the test results
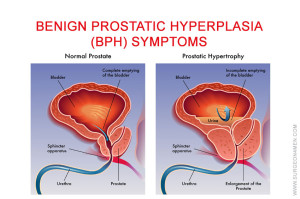
- Medications used for treating benign prostate hyperplasia such as Finasteride can also alter the result.
What to Think
- The sensitivity for diagnosing prostate cancer increases with digital rectal exam
- Some men with existing prostate malignancy may sometimes show normal PSA results (within normal ranges)
- In case of raised levels of PSA, the physician must obtain confirmatory tests before making the final diagnosis of prostate malignancy, Age and health status of a person should also be considered before making the diagnosis.
For differentiating between benign prostate hyperplasia and prostate cancer following tests are performed,
- PSAD (Prostate Specific Antigen Density):In which the size of prostate gland is compared with corresponding PSA levels.
- PSA Velocity Test: In which the rise in the concentration of PSA levels is assessed with respect to time.
- c-PSA (Complexed Prostate Specific Antigen): To measure various forms of PSA to ascertain the need for additional testing.
References:
- Cooper, C. P., Merritt, T. L., Ross, L. E., John, L. V., & Jorgensen, C. M. (2004). To screen or not to screen, when clinical guidelines disagree: primary care physicians’ use of the PSA test. Preventive medicine, 38(2), 182-191.
- Carlsson, S., Aus, G., Wessman, C., & Hugosson, J. (2007). Anxiety associated with prostate cancer screening with special reference to men with a positive screening test (elevated PSA)–Results from a prospective, population-based, randomised study. European Journal of Cancer, 43(14), 2109-2116.
- Legler, J. M., Feuer, E. J., Potosky, A. L., Merrill, R. M., & Kramer, B. S. (1998). The role of prostate-specific antigen (PSA) testing patterns in the recent prostate cancer incidence declinein the United States. Cancer Causes & Control, 9(5), 519-527.